


解剖性肺段切除术在早期肺癌的治疗中扮演越来越重要的角色,但同时对术者的专业技能要求更高。近年来,福建医科大学附属协和医院副院长陈椿教授团队在肺部结节的定位、段间静脉的处理、肺段平面的辨识等多个关键技术环节提出了具有中心特色的实践经验,可操作性强,实用性高。
近期,由福建医科大学附属协和医院以及来自美国、日本、德国、瑞士五个国家医院的胸外科、16位专家所组成的AME胸外科协作组在国际肺癌转化研究专刊《Translational Lung Cancer Research》发表题为“Management of the inter-segmental plane using the ‘Combined Dimensional Reduction Method’ is safe and viable in uniport video-assisted thoracoscopic pulmonary segmentectomy”(单孔胸腔镜肺段切除术中采用“联合降维法”处理肺段间平面的安全可行性研究)的临床研究论文,协作组应用医达健康IQQA精准手术规划平台对220例胸腔镜肺段切除术患者进行术前精准评估及手术规划,以规模性临床研究病例得出结论:联合降维法有助于提高单孔腔镜肺段切除术的便捷性和精准性,是一种安全有效的方法,值得在临床推广应用。
此外,陈椿教授团队还在《中华胸部外科电子杂志》发表了题为“联合降维法在达芬奇机器人辅助精准肺段切除术中的应用”论文,详细介绍了首例将IQQA精准手术规划平台与达芬奇机器人系统结合,在联合降维法的理论方法下完成的精准复杂肺段切除治疗早期肺癌的成功经验,该方法有助于提高肺段切除的精准性,借助机器人高清晰的分辨率、三维的视觉展示提高手术的安全性,二者的联合应用对肺段切除的个体化、智能化均有重要意义。
1

原文链接:http://tlcr.amegroups.com/article/view/32458/22819
Background: The management of the intersegmental plane (ISP) is challenging during uniport video-assisted thoracoscopic (VATS) pulmonary segmentectomy. Staplers and electrocautery have been used extensively in ISP management. However, both of them have their respective drawbacks. Currently, we have provided a revised technique termed as “Combined Dimensional Reduction Method” (CDR method), for managing the ISP with combined application of ultrasonic scalpel and staplers. The study aimed to review the outcomes of patients who underwent uniport VATS segmentectomy with or without the CDR method in our institute and assess the feasibility and safety of the CDR method.
Methods: From March 2017 to February 2018, 220 patients who underwent uniport VATS segmentectomy were retrospectively reviewed. By using IQQA software, pulmonary structures were reconstructed as three-dimensional (3D) images, making the targeted structures could be identified preoperatively. For the management of the ISP, in the CDR group, we firstly used the ultrasonic scalpel to trim the 3D pulmonary structure along the intersegmental demarcation, making the remaining targeted parenchyma both sufficiently thin enough and located on a 2D plane; thus, enabling easy use of staplers in managing ISP. Whereas, in the non-CDR group, we only use the staplers to manage the ISPs. The clinical characteristics, complications, and postoperative pulmonary functions were compared between the two groups.
Artificial intelligence-assisted mapping planning
CT images were obtained using 64-slice spiral CT scanner GE Light Speed VCT with a slice thickness of 1.25 mm. Both non-enhanced and contrast-enhanced scans were performed. CT data of all patients were stored in the DICOM format. In both groups, the data for all patients were imported in the IQQA-3D (EDDA Technology, Princeton, NJ, USA). The software automatically recognizes the pulmonary structures and reconstructs the three-dimensional (3D) pulmonary structures of the bronchial tree, arteries, and veins. The small number of differences between the reconstructed structures and two-dimensional (2D) CT images were manually reconciled. After reconstruction, the data were saved as still images and dynamic videos. Measured 2D data, including diameters of lesions and structures, along with lengths and the angles of branches of vessels and bronchi, were determined by measurement tools in IQQA. The positional relationship between lesions and the segmental structures were defined, and the possible variant segmental structures were analyzed. Virtual surgery was performed on the reconstructed dynamic 3D model (Figure 1), and the remaining pulmonary volume was calculated to evaluate the feasibility of the proposed operation strategies. The treatment plan was finally defined after optimization of the individualized virtual surgery.
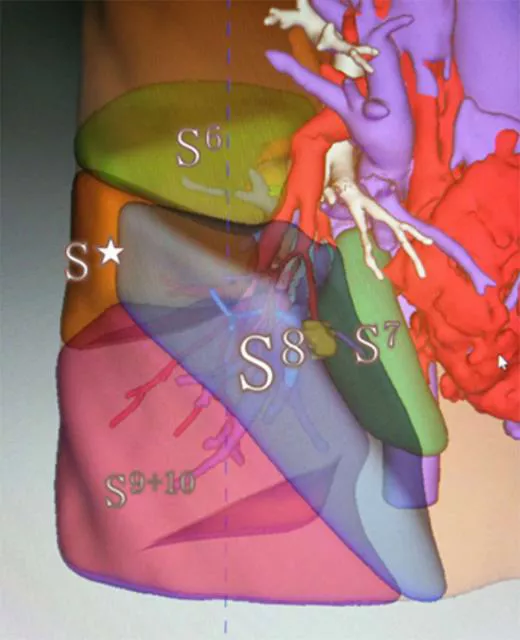
Figure 1 Virtual surgery was performed on the reconstructed dynamic 3D model (take RS8 as an example). All 2D data of segmental structures were analyzed, including the location, length, number of branches, diameter of branches, and angle of branches. S* means subsuperior segment.
Results: Propensity score analysis generated 2 well-matched pairs of 71 patients in CDR and non-CDR groups. There was no 30-day postoperative death or readmission in either group. The CDR group was significantly associated with the shorter operative time (178.3±35.8 vs. 209.2±28.7 min) (P=0.031) and postoperative stay (4.5±2.3 vs. 5.7±4.2 days) (P=0.041), compared to the non-CDR group. Moreover, no significant difference was observed in blood loss, a period of chest tube drainage, a period of ultrafine tube drainage, and postoperative pulmonary complications between the two groups. Moreover, the recovery rate of postoperative forced expiratory volume in 1 second (FEV1) or vital capacity (VC) at 1 and 3 months after segmentectomy was comparable between them.
Conclusions: The CDR method could make segmentectomy easier and more accurate, and therefore has the potential to be a viable and effective technique for uniport VATS pulmonary segmentectomy.
2
联合降维法在达芬奇机器人辅助精准肺段切除术中的应用
作者:张树亮,郑斌,徐国兵,郑炜,陈椿
《中华胸部外科电子杂志》2019年第6卷第2期
患者,女,32岁。以“体检发现右下肺结节1年余”为主诉。入院后行肺部薄层CT检查提示:右肺下叶(S3I39)见一小结节影,直径约0.5cm,边界尚清,与体检时肺部CT影像相仿(图1)。临床诊断为右下肺结节性质待查:肺癌可疑。
联合降维法:术前将2D影像资料通过IQQA精准手术规划平台处理成为3D立体结构;术中将段间3D结构通过超声刀及电钩沿段间平面分离成一平面,将3D的立体结构降维成2D的平面结构,然后用直线切割缝合器处理。这样既可以保证靶肺段的精准切除又可以使余肺舒展、膨胀良好,最大限度减少肺功能损失。
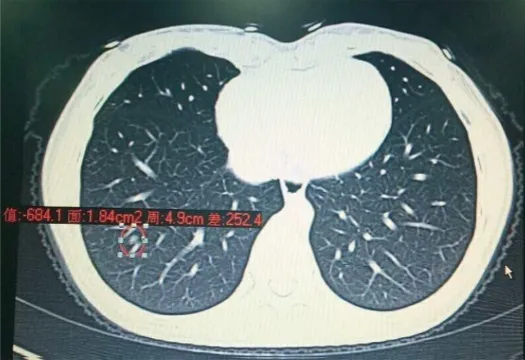
图1 患者入院肺部薄层CT检查结果
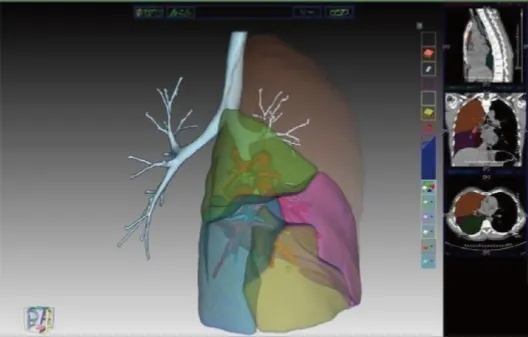
图2 IQQA平台对患者肺部结构进行分析并精确定位(黄色点即为肿瘤)

图3 达芬奇机器人系统行段间平面的精准处理
临床总结:“结合笔者的临床经验,在联合降维法的理论下行肺段切除可以取得较好的效果。IQQA精准手术规划平台可以依据肺内气管、肺动脉、肺静脉的走行,利用2D和3D立体切面,细致而准确地划分肺段,进一步立体化显示病灶累及肺段范围。该平台可以将病灶精确定位到亚段水平,可以显示病灶周围细微的局部解剖,进一步缩小手术切除范围,从而最大限度地保留肺功能。其次,IQQA平台可以为临床医师提供准确的气管支气管、靶段血管3D模式图,图像立体感强、对比鲜明,可以准确描绘肺内,特别是肿瘤相关空间的血管分布,为下一步制定模拟手术做好充足准备。再次,IQQA平台具有模拟手术功能,可以虚拟离断靶段肺静脉以及靶段肺动脉,为外科医师设计和优化手术方案提供客观的图形化的决策依据。另外,IQQA平台最为突出的优势在于可为手术方案制定提供十分重要的量化信息,诸如病灶体积、各肺段边界等。在模拟肺段切除术基础上,计算术后剩余具有功能的肺脏体积,结合术前肺功能,可以更加准确地预估术后残余肺功能,个性化制定并修正手术方案。特别是对于老年、肺功能差无法耐受肺叶切除但可以承受肺段或亚段切除的患者,使其获得最大手术收益。术中再将3D立体结构通过精细解剖为2D平面再予以直线切割缝合器处理,这样可以完整地切除靶肺段,又最大限度保留余肺组织;既可以有效地控制创面渗血及漏气等并发症,又可以较好地保持余肺创面舒张,避免创面因缝合造成的卷曲及膨胀不良。结合本例的成功经验来看,联合降维法能够在精准肺段切除中取得较好的效果,加强胸外科一线医疗工作者外科手术微创化理念,并有利于患者减少手术创伤,加速术后恢复。”